Persistent aches in hips or spine may reflect leaching calcium reserves. Parathyroid hormone (PTH) dysregulation weakens bone density over years. Fractures occur with minimal trauma. Delayed healing follows. X-rays show moth-eaten bone patterns.
Kidney stones recur despite hydration efforts
Excess calcium excreted through urine crystallizes into painful stones. High PTH increases renal calcium waste. Ultrasound reveals calcifications in kidneys. Dietary adjustments alone rarely resolve this.
Muscle cramps hint at electrolyte chaos
Low calcium triggers involuntary spasms in hands, feet, or face. Tingling precedes full cramps. Serum calcium levels dip below 8.5 mg/dL. Magnesium deficiency often coexists. Intravenous calcium stops acute episodes.
Fatigue isn’t laziness—it’s metabolic sabotage
Chronic hypocalcemia slows cellular energy production. ATP synthesis falters. Patients nap frequently but wake unrefreshed. Thyroid tests appear normal, masking parathyroid links.
Hyperparathyroidism often hides behind “normal” lab ranges
PTH levels slightly above reference limits escape notice. Ionized calcium tests uncover subtle elevations. Asymptomatic cases progress silently for years. Delayed surgery risks irreversible organ damage.
Neck surgeries accidentally remove parathyroid glands
Thyroid operations damage tiny parathyroid glands in 3% of cases. Sudden hypocalcemia requires lifelong supplements. Intraoperative PTH monitoring reduces this risk.
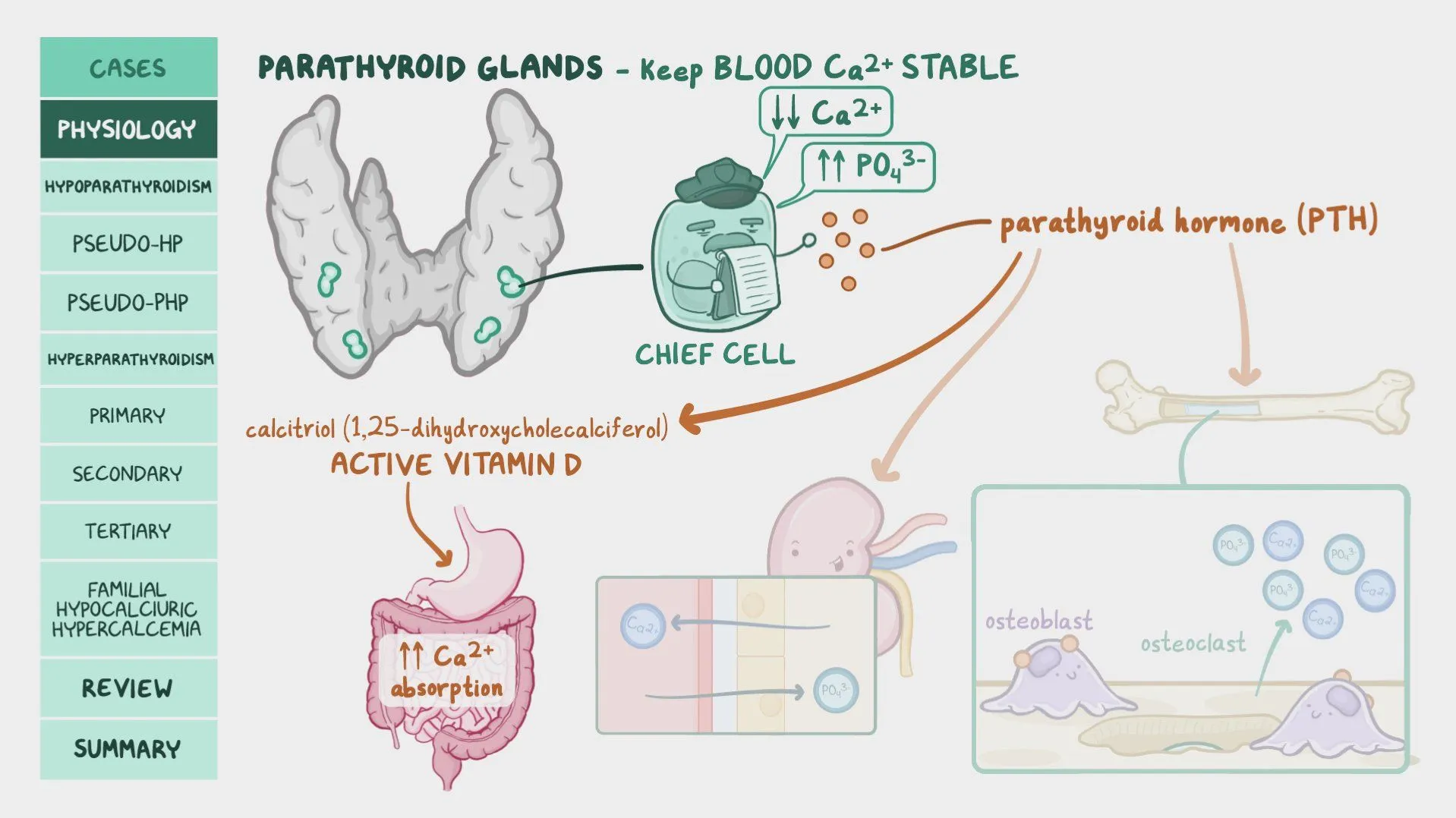
Vitamin D deficiency masks root causes
Low vitamin D skews calcium and PTH readings. Repleting vitamin D unmasks hidden hyperparathyroidism. Testing both nutrients together clarifies diagnoses.
Hungry bone syndrome drains calcium post-surgery
After parathyroidectomy, bones rapidly absorb calcium from blood. Levels crash despite supplements. Intravenous infusions prevent life-threatening tetany. Monitoring continues for weeks.
Genetic mutations predispose families to disorders
MEN syndromes link parathyroid tumors to pituitary/pancreatic issues. Genetic testing guides screening for relatives. Early intervention prevents multisystem crises.
Calcium-sensing receptor defects mimic imbalances
Mutated receptors misread calcium levels, causing inappropriate PTH secretion. Cinacalcet adjusts receptor sensitivity. Diagnosing this avoids unnecessary surgeries.
Pseudohypoparathyroidism resists standard treatments
Kidneys ignore PTH due to receptor defects. Calcium and vitamin D doses exceed typical needs. Specialty labs confirm this rare disorder.
Parathyroid cancer is rare but aggressive
Rapid calcium spikes above 14 mg/dL demand imaging. Surgery removes malignant glands. Recurrence rates hit 50% within five years.
Osteoporosis drugs fail if PTH isn’t controlled
Bisphosphonates can’t rebuild bones while PTH drains calcium. Dual-energy X-ray scans track density changes. Correcting PTH comes first.
Pregnancy strains calcium-PTH equilibrium
Fetal demands double maternal calcium needs. Uncontrolled hyperparathyroidism risks preeclampsia. Careful monitoring balances fetal growth and maternal safety.
Dialysis patients battle secondary hyperparathyroidism
Failed kidneys can’t excrete phosphate, raising PTH. Calcimimetics reduce hormone levels. Unmanaged cases lead to cardiovascular calcification.
Voice changes may signal gland enlargement
Enlarged parathyroids press on laryngeal nerves. Hoarseness develops gradually. Neck ultrasounds differentiate nodules from thyroid issues.
Mental fog stems from neuronal instability
Calcium fluctuations disrupt neurotransmitter release. Memory lapses and irritability worsen with stress. Restoring levels sharpens cognition.
GI symptoms overlap with common disorders
Constipation, nausea, or reflux mimic IBS. Hypercalcemia slows gut motility. Correcting calcium eases digestion without antacids.
Cardiac arrhythmias escalate with calcium swings
Prolonged QT intervals on EKGs signal danger. Calcium stabilizes heart rhythms. Emergency IV infusions prevent cardiac arrest.
Urine calcium tests predict stone recurrence
24-hour collections exceeding 250 mg warn of hyperparathyroidism. Low citrate levels compound risk. Dietary citrate supplements help.
Parathyroid cysts are rare but symptomatic
Large cysts compress nearby structures, causing swallowing difficulties. Aspiration provides temporary relief. Surgical removal is definitive.
Alcoholism exacerbates calcium-PTH dysregulation
Chronic drinking lowers magnesium, skewing PTH secretion. Repletion improves hormone responsiveness. Relapse risks recurrence.
Steroid use masks calcium imbalances
Glucocorticoids lower intestinal calcium absorption. Compensatory PTH rises hide underlying issues. Bone density scans reveal hidden damage.
Lithium therapy triggers gland overactivity
Long-term use enlarges parathyroids in 15% of patients. Regular calcium checks prevent severe hypercalcemia.
Aging silently disrupts calcium homeostasis
Postmenopausal women face doubled hyperparathyroidism rates. Routine screenings after 50 catch subtle shifts early.
False lab results delay correct diagnoses
Hemolysis or improper sample handling alters calcium readings. Repeating tests with fasting samples clarifies truth.
Non-parathyroid cancers mimic hormone excess
Lung or breast tumors secrete PTH-related protein. Imaging locates ectopic sources. Treatment focuses on primary cancer.
Custom calcium protocols prevent crises
Dosing varies by absorption capacity and kidney function. Compounded formulas suit individual needs. Regular labs fine-tune regimens.